Athletic Training Services
Craig High School Athletic Trainer - Kathy Calkins, LAT
Janesville Craig Athletic Trainer, Kathy Calkins, LAT, has athletic training room hours at Craig most days from 2:30pm to 5:30pm. This changes depending on the athletic contests that may be occurring that day. An up-to-date schedule is posted on the calendar on the athletic training room door (room 200, across from the athletic concession stand).
The athletic training room is located in Room 200 which is located directly across from the concession stand between the fieldhouse and the main gym.
All students are eligible to enroll into the STUDENT ACCIDENT INSURANCE PROGRAM through Student Assurance Services. There is a one-time premium for the entire school year. For more information, visit www.sas-mn.com. To enroll, visit:
https://www.janesville.k12.wi.us/departments/athletics/forms-and-registration-information
or
The HeadStrong Concussion Insurance Program, created by the WIAA, was specifically developed to insure your student-athlete from the potential high cost of concussion treatment and follow-up that may be required after a suspected concussion. Coverage is secondary to/in excess of any other valid and collectible insurance but will be the primary payor if no other insurance is available. This only applies to WIAA student-athletes and the concussion has to occur while in WIAA sanctioned activity during this time-frame. For more information: https://www.wiaawi.org/Health/Concussion-and-Sudden-Cardiac-Arrest-Information/Concussion-Insurance
- This form is REQUIRED to be eligible to wrestle if there is a suspected skin condition such as ringworm or impetigo. Be sure to take this form with you to the doctor https://www.wiaawi.org/Portals/0/PDF/Sports/Wrestling/wrestrelease.pdf
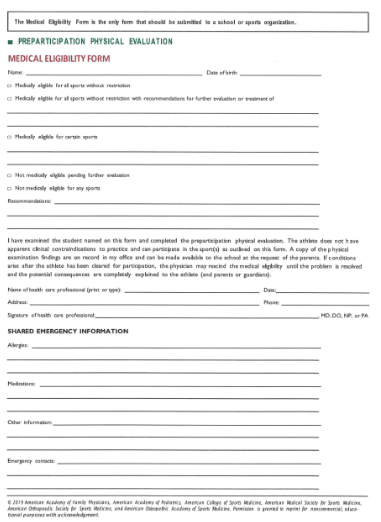
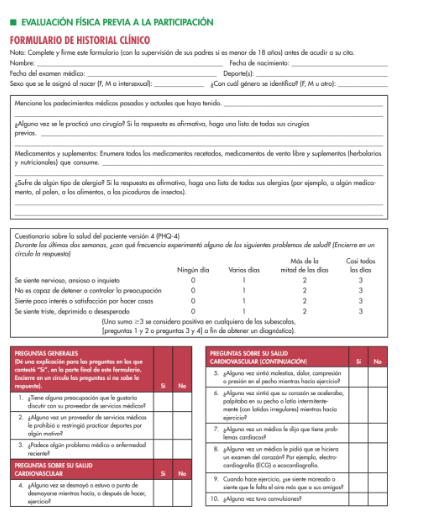
- Yes. A Current Sports Physical, signed and dated by the doctor, must be on file in the Athletic Office. NOTE: To participate in the 2025-2026 school year, your physical date must be 4/1/2024 or after. Physicals can be dropped off in the Athletic Office, faxed to 608.743.5196 or a copy emailed to the athletics secretary.
Wisconsin State Concussion Law (Act 172) mandates that if an athlete exhibits any of the signs, symptoms, or behavior consistent with a concussion or head injury OR you simply suspect the person has sustained a concussion or head injury, the athlete must be removed from all physical activity immediately, and must complete the 6 Step Return To Play Protocol. The athlete will not be allowed to return to practice or competition until they have completed all aspects of the return to play protocol and been cleared by a healthcare professional trained in the management of concussions.
JSD students who think they may have a concussion should notify their coach AND athletic trainer as soon as possible. The athletic trainer will complete a concussion evaluation and monitor the athlete throughout the gradual return to activity concussion protocol. The School District of Janesville follows standard return to play recommendations. From the WIAA website:
The program described below is a guideline for returning concussed student-athletes when they are symptom free. Student-athletes with multiple concussions and athletes with prolonged symptoms often require a prolonged or different return to activity program and should be managed by a physician that has experience in treating concussion.
The following program allows for one step per 24 hours. The program allows for a gradual increase in heart rate/physical exertion, coordination, and then allows contact. If symptoms return, the athlete should stop activity and notify their healthcare provider before progressing to the next level.
STAGE ONE: Daily activities that do not increase symptoms (gradual reintroduction of school, work and walking).
STAGE TWO: Light aerobic exercise: slow to medium pace jogging, stationary cycling. No resistance training. No increase in symptoms. This stage allows for increased heart rate – begin with <55% of max HR, but if tolerating, can progress to <70% of max HR.
STAGE THREE: Sport-specific exercise: moderate to higher intensity running or skating drills, but no activities with risk of head impact. This allows for increased heart rate and agility/movement.
STAGES 4-6 should only begin after the resolution of any symptoms, abnormalities in cognitive function, and any other clinical finding related to the current concussion, including during and after physical exertion.
STAGE FOUR: Non-contact training: Higher intensity aerobic fitness, and non-contact/non-collision team training drills (e.g., passing drills). May begin progressive resistance training. This increases coordination and thinking during sport.
STAGE FIVE: Full contact practice. Written medical clearance is required to resume contact or high-risk activity, allowing the athlete to participate fully in normal training activities. This restores confidence and allows coaches to assess functional skills.
STAGE SIX: Full clearance / Normal game play.
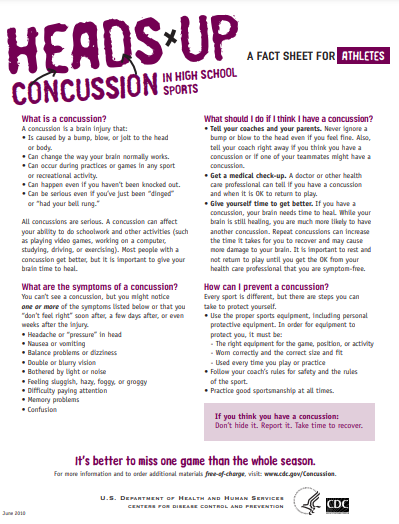
Fact Sheets from CDC for High School Athletes regarding concussions: https://www.cdc.gov/headsup/pdfs/highschoolsports/athletes_fact_sheet-508.pdf
A concussion is a type of brain injury that changes the way the brain normally works. A concussion is caused by a bump, blow, or jolt to the head. Concussions can also occur from a blow to the body that causes the head and brain to move rapidly back and forth. Even what seems to be a mild bump to the head can be serious.
Concussions can have a more serious effect on a young, developing brain and need to be addressed correctly.
What are the signs and symptoms of a concussion?
You can’t see a concussion. Signs and symptoms of concussion can show up right after an injury or may not appear or be noticed until hours or days after the injury. It is important to watch for changes in how your child or teen is acting or feeling, if symptoms are getting worse, or if s/he just “doesn’t feel right.” Most concussions occur without loss of consciousness.
If your child or teen reports one or more of the symptoms of concussion listed below, or if you notice the symptoms yourself, seek medical attention right away. Children and teens are among those at greatest risk for concussion.
| Signs Observed by Parents or Guardians | Symptoms Reported by your Child or Teen Thinking/Remembering: | Symptoms Reported by your Child or Teen Emotional: |
|---|---|---|
|
Physical:
|
Sleep:
|
To download this fact sheet in Spanish, please visit: www.cdc.gov/Concussion.
DANGER SIGNS
Be alert for symptoms that worsen over time. Your child or teen should be seen in an emergency department right away if s/he has:
- One pupil (the black part in the middle of the eye) larger than the other
- Drowsiness or cannot be awakened
- A headache that gets worse and does not go away
- Weakness, numbness, or decreased coordination
- Repeated vomiting or nausea
- Slurred speech
- Convulsions or seizures
- Difficulty recognizing people or places
- Increasing confusion, restlessness, or agitation
- Unusual behavior
- Loss of consciousness (even a brief loss of consciousness should be taken seriously)
Children and teens with a concussion should NEVER return to sports or recreation activities on the same day the injury occurred. They should delay returning to their activities until a health care professional experienced in evaluating for concussion says they are symptom-free and it’s OK to return to play. This means, until permitted, not returning to:
- Physical Education (PE) class,
- Sports practices or games, or
- Physical activity at recess.
- Seek medical attention right away. A health care professional experienced in evaluating for concussion can determine how serious the concussion is and when it is safe for your child or teen to return to normal activities, including physical activity and school (concentration and learning activities).
- Help them take time to get better. If your child or teen has a concussion, her or his brain needs time to heal. Your child or teen may need to limit activities while s/he is recovering from a concussion. Exercising or activities that involve a lot of concentration, such as studying, working on the computer, or playing video games may cause concussion symptoms (such as headache or tiredness) to reappear or get worse. After a concussion, physical and cognitive activities—such as concentration and learning—should be carefully managed and monitored by a health care professional.
- Together with your child or teen, learn more about concussions. Talk about the potential long-term effects of concussion and the dangers of returning too soon to normal activities (especially physical activity and learning/concentration). For more information about concussion and free resources, visit: www.cdc.gov/Concussion.
Help your child or teen get needed support when returning to school after a concussion. Talk with your child’s teachers, school nurse, coach, speechlanguage pathologist, or counselor about your child’s concussion and symptoms. Your child may feel frustrated, sad, and even angry because s/he cannot return to recreation and sports right away, or cannot keep up with schoolwork. Your child may also feel isolated from peers and social networks. Talk often with your child about these issues and offer your support and encouragement. As your child’s symptoms decrease, the extra help or support can be removed gradually. Children and teens who return to school after a concussion may need to:
- Take rest breaks as needed,
- Spend fewer hours at school,
- Be given more time to take tests or complete assignments,
- Receive help with schoolwork, and/or
- Reduce time spent reading, writing, or on the computer.
To learn more about concussion and to order materials FREE-OF-CHARGE, go to: www.cdc.gov/Concussion or call 1.800.CDC.INFO.
You can’t see a concussion. Signs and symptoms of concussion can show up right after an injury or may not appear or be noticed until hours or days after the injury. It is important to watch for changes in how your child or teen is acting or feeling, if symptoms are getting worse, or if s/he just “doesn’t feel right.” Most concussions occur without loss of consciousness.
If your child or teen reports one or more of the symptoms of concussion listed below, or if you notice the symptoms yourself, seek medical attention right away. Children and teens are among those at greatest risk for concussion.
| Signs Observed by Parents or Guardians | Symptoms Reported by your Child or Teen Thinking/Remembering: | Symptoms Reported by your Child or Teen Emotional: |
|---|---|---|
|
Physical:
|
Sleep:
|
To download this fact sheet in Spanish, please visit: www.cdc.gov/Concussion.
DANGER SIGNS
Be alert for symptoms that worsen over time. Your child or teen should be seen in an emergency department right away if s/he has:
- One pupil (the black part in the middle of the eye) larger than the other
- Drowsiness or cannot be awakened
- A headache that gets worse and does not go away
- Weakness, numbness, or decreased coordination
- Repeated vomiting or nausea
- Slurred speech
- Convulsions or seizures
- Difficulty recognizing people or places
- Increasing confusion, restlessness, or agitation
- Unusual behavior
- Loss of consciousness (even a brief loss of consciousness should be taken seriously)
Children and teens with a concussion should NEVER return to sports or recreation activities on the same day the injury occurred. They should delay returning to their activities until a health care professional experienced in evaluating for concussion says they are symptom-free and it’s OK to return to play. This means, until permitted, not returning to:
- Physical Education (PE) class,
- Sports practices or games, or
- Physical activity at recess.

1st Team Award Winner
Janesville Craig High School has received the National Athletic Trainers’ Association (NATA) Safe Sports School Award since 2020. The award champions safety and recognizes secondary schools that have met the recommended standards to improve safety in sports. The award reinforces the importance of providing the best level of care, injury prevention, and treatment.
To apply, schools complete an in-depth questionnaire that assesses adherence to best practice standards and recommendations. For more information about the Safe Sports School Award, please visit www.athletictrainers.org
“Janesville Craig is honored to receive this 1st Team recognition from NATA,” said Ben McCormick, Craig’s athletic director. “We remain committed to keeping our student athletes safe during physical education classes, team practices, and games so they can accomplish their own goals of great competition, winning records, fair sportsmanship, and good health. Our goal is to lead our athletics program to the highest safety standards for our players.”
Ben McCormick, CAA
Athletics & Activities Director, Craig High School

“The health and safety of student athletes is critical as it has both immediate and long-term effects. “The National Athletic Trainers’ Association created the ‘Safe Sports School Award’ to recognize and champion schools nationwide that are committed to safety in sports. We are proud to see the list of award recipients grow exponentially each year as schools see the immense value in holding themselves to best practices and policies that ensure a high standard of athlete care.”
Kathy Dieringer, EdD, LAT, ATC
President, National Athletic Trainers' Association